Study evaluates college football players’ positions for risk of concussions
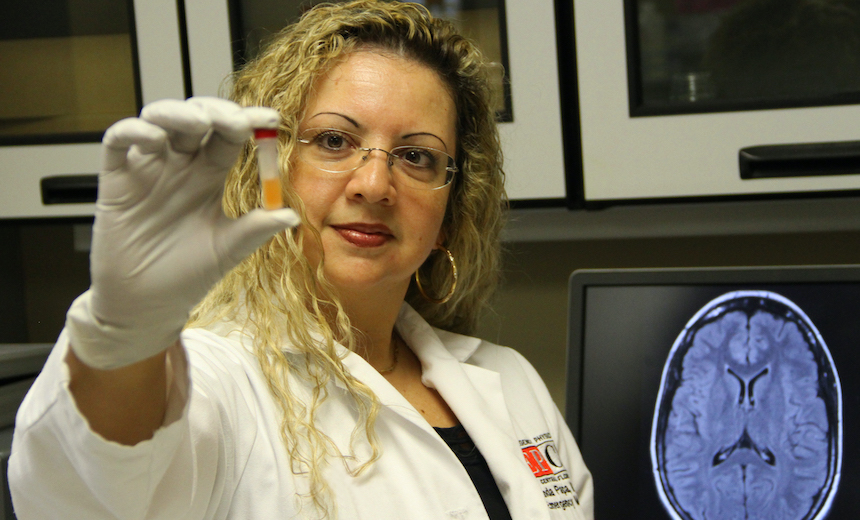
An Orlando Health Orlando Regional Medical Center (ORMC) researcher is the lead author of a new study, published in the Journal of Neurotrauma, that reveals elevated traumatic brain injury biomarkers in football players in skill positions.
Orlando, Fla. (September 22, 2022) — A new research study looks inside the brains of college football athletes to measure levels of traumatic brain injury (TBI) biomarkers by player position. This study, conducted in collaboration with researchers at Orlando Health Orlando Regional Medical Center (ORMC) and Penn State University, and published in the Journal of Neurotrauma, sheds light on which positions are at the greatest risk for elevations in brain injury biomarkers. The biomarkers are proteins and other substances released from the brain after it has been damaged.
Researchers followed 52 college football athletes, pre-season and post-season, and measured four biomarkers (glial fibrillary acidic protein [GFAP], ubiquitin C-terminal hydrolase-L1 [UCH-L1], total Tau, and neurofilament light chain polypeptide [NF-L]). The players were grouped by two established classification systems: speed versus non-speed positions, and Profile 1, Profile 2, and Profile 3.
“We found the biomarkers were much higher in football players in speed positions such as quarterbacks, wide receivers, defensive backs, running backs, halfbacks, fullbacks, tight ends, defensive backs, safety, and linebackers who build up momentum prior to tackling or being tackled, compared to non-speed positions like offensive and defensive linemen who engage other players before significant momentum can be generated,” said Linda Papa, MD, lead author of the study and emergency medicine physician and director, Academic Clinical Research, Orlando Health ORMC. “Interestingly, biomarkers increased in all positions over the course of the season despite very few players being diagnosed with a concussion. This suggests that repetitive head impact exposures elevate TBI biomarkers without having a concussion.”
Furthermore, Papa and colleagues used a three-tier player position classification system developed by researchers using biomechanical measurements including head impact strain magnitude, head impact frequency and intervals. Profile 1 positions are those who receive high intensity hits, but not often (termed high strain magnitudes/low frequency by the researchers). These positions include quarterbacks, wide receivers, and defensive backs. Profile 2 positions are mid-range impact frequency and strain positions including linebackers, running backs, and tight ends. Profile 3 positions are those who are hit often, but the hits are of lower intensity (low strain magnitude/high frequency) and include defensive and offensive linemen.
“It appears that head impact magnitude and not frequency causes the greatest elevations in TBI biomarkers,” said Dr. Papa. “We found incremental increases in the biomarkers GFAP, Tau, and NF-L by player position from Profile 3 to Profile 2 to Profile 1, with highest biomarker levels in Profile 1 players and lowest biomarker levels in Profile 3 players.”
An unexpected finding was that the biomarker elevation patterns in speed (and Profile 1) versus non-speed (and Profile 3) players were not only present at the end of the season but also before the season began. “This was surprising because blood was collected before any practices or football activity,” said Linda Papa. “It may indicate that pre-season biomarker elevations in these players reflect head impact exposures from previous seasons.”
The study, which combines TBI biomarkers in blood with established player classifications systems (based on biomechanical measurements) across pre- and post-seasons, is among the first of its kind.
“Measuring TBI biomarkers in blood could potentially offer an objective and relatively simple way of quantifying and monitoring head impact exposures in different players,” said Dr. Papa.
Understanding TBI biomarker changes by player position can be helpful in considering safety measures, game rule changes, on-field behavior, enhancements to equipment, return-to-play guidance, career decisions, and other factors.
Future evaluation of a larger sample of players over a longer period of time, could reveal more information and provide greater understanding about the long-term impact of traumatic brain injuries associated with player positions, said Dr. Papa.
Researchers at Orlando Health ORMC were leaders in identifying GFAP and UCH-L1 – the two FDA-approved biomarkers used in blood testing to detect brain injury and have continued to evaluate different aspects of the biomarkers through various studies. Dr. Papa, who has 20 years of experience in traumatic brain injury biomarkers research, has been the lead author of many studies published in various publications including JAMA Network Open, JAMA Neurology, BMJ Paediatrics Open, Academic Emergency Medicine, and Journal of Trauma. Dr. Papa has published more than 200 articles related to traumatic brain injury.
About Orlando Health
Orlando Health, headquartered in Orlando, Florida, is a not-for-profit healthcare organization with $8 billion of assets under management that serves the southeastern United States.
Founded more than 100 years ago, the healthcare system is recognized around the world for Central Florida’s only pediatric and adult Level One Trauma program as well as the only state-accredited Level Two Adult Trauma Center in the St. Petersburg region. It is the home of the nation’s largest neonatal intensive care unit under one roof, the only system in the southeast to offer open fetal surgery to repair the most severe forms of spina bifida, the site of an Olympic athlete training facility and operator of one of the largest and highest performing clinically integrated networks in the region. Orlando Health has pioneered life-changing medical research and its Graduate Medical Education program hosts more than 350 residents and fellows. The 3,200-bed system includes 10 award-winning hospitals, 9 hospital-based ERs, and 7 free-standing emergency rooms; rehabilitation services, cancer and heart institutes, imaging and laboratory services, wound care centers, physician offices for adults and pediatrics, skilled nursing facilities, an in-patient behavioral health facility, home healthcare services in partnership with LHC Group, and urgent care centers in partnership with FastMed Urgent Care. More than 4,200 physicians, representing more than 100 medical specialties and subspecialties have privileges across the Orlando Health system, which employs more than 23,000 team members. In FY21, Orlando Health served more than 160,000 inpatients and 3.6 million outpatients. During that same time period, Orlando Health provided approximately $648 million in total value to the communities it serves in the form of charity care, community benefit programs and services, community building activities and more. Additional information can be found at http://www.orlandohealth.com, or follow us on LinkedIn, Facebook, Instagram and Twitter @orlandohealth.








