Wellness and Resilience Strategies During Covid-19
COVID-19 has been a critical incident that impacted everyone around the world, and it created uncertainty and a sense of powerless for many individuals. Healthcare workers have been in the forefront of this pandemic and the impact has been cumulative and wide-ranging. Therefore, we have created this handout titled Wellness Tips that you can download and share.
Additionally, we have engaged in an ongoing process of writing very brief articles packed with information, tips, and strategies that you will find below.
-
Adapting Through Crisis +
The title of this article is purposeful. Crises are not events to get over, but events one must learn to work through. Adaptability is a skill that has been proven to be one of the greatest contributing factors to wellbeing during times of crises. Research conducted in the areas of performance, burnout, uncertainty yielded the concept of Adaptability Quotient (AQ). Although many are familiar with the concept of IQ as it relates to intelligence, AQ has gained notoriety, especially during our current times. It refers to the ability to adjust, change, and even shifting your thinking to one that fits the current situation, but more importantly, with a focus on what is beyond the horizon.
It is widely known that healthcare has been rapidly changing; however, the current situation has caused the healthcare system to reinvent itself, causing health systems to evaluate their models and adjust to the current needs as well as figure out a way to predict future outcomes. As a vital part of any healthcare system, the contributions, ideas, and wellbeing of its physicians is crucial as the organization adapts to what the future holds. Here are a few ways for you to increase your own AQ as well as continue to support the organization:
· Seek Opportunities. Those with high AQ approach unprecedented times as sources of unprecedented opportunities. We are living in a situation we have never experienced before. Therefore, old models may not work and being innovative about ways to capitalize on the new healthcare gaps can be important.
· Be Resourceful. There is a difference between resources and resourcefulness. When resources are scarce or can potentially run low, resourcefulness can be driven by creativity, collaboration, and new relationships.
· Remain Engaged. As noted in the previous tip, new collaborations and relationships are often born out of necessity. Therefore, stay informed with current updates, ask questions, attend meetings, and continue to see yourself as an important part of the organization.
· Share Your Ideas. Inform your colleagues and teams of ideas you believe can help. They will listen to you and the organization values everyone’s ideas and there is a potential for your idea to be put into action or added to a more collective idea that had already been in the works.
· Come to Terms with the New Normal. Crises, personal as well as collective ones, causes individuals to adjust to a new normal. It is important to work through the way “things used to be” because when we start to come out of this, many systems, protocols, and even interactions will be different. The hope is that most will be more efficient, effective and empowered.
-
Adding Value to Others +
One recommendation that has been established to mitigate the spread of COVID-19 has been social distancing. This practice has provided opportunities for individuals as well as organizations to develop creative ways to stay connected. The current situation can be used as a time to re-evaluate what is important, re-define boundaries, and re-discover connections. Here are a few strategies to make the add value to others during what we are facing:
· Reach Out to Others. Reach out to others whom you have not talked to in a while. The current situation gives you the perfect “excuse” to do so, and it will help you expand your support system. It might also re-connect you with parts of you, your history, and your culture that will add value to your life.
· Give to Others in Need. Right now, many individuals, including team members, are struggling with financial losses and even loss of employment. If you have the financial resources, help someone out, even if it is something that seems small. Anything counts during these times. However, it does not have to be finances, it could be giving of your time and talent. For instances, if you are very good with a school subject, you could give 30 minutes of free tutoring to a family who is homeschooling their child. You never know who you could inspire and influence by giving and connecting with others under these circumstances.
· Share Meaningful Videos. Right now, individuals are connected and engaged in social media at greater rates. However, those platforms are inundated with COVID-19 news and reports. You can post a TED talk or another video that has been an inspiration to you. Thus, disrupting the endless cycle of feeds and posts related to the current situation.
-
Communication with Your Team +
A key aspect during challenging situations is communication with your team. Communication can help or hinder the way a team functions, works through, and recovers from difficult events. Even the best communicators can find it demanding because of the amount of information, as well as how rapid it is changing; not to mention the team you work with might have different needs based on their roles, functions, and even personalities.
Keeping in mind the importance of communication is the first step in enhancing the effectiveness and impact of your messages to them. During uncertain times, individuals’ capacity to receive and process information is compromised. Therefore, how you communicate the information is more important than what you communicate. Here are a few tips:
· Focus on the Gains. When providing information or facts, focus on what is being accomplished and what the results have been by framing them as gains. For instance, instead of telling them that 9% of patients are testing positive, it is better to tell them that 91% are testing negative. This is an example to illustrate the principle you can use in your respective unit/department when providing information. Positive information (gains and accomplishments) helps individuals cope and process content better.
· Keep it Brief. It is more helpful to provide information that is concise and specific to the question(s). Providing excessive information can create more confusion, and even frustration in your team members.
· Send Summary Email. Although the organization is doing a superb job in keeping everyone informed, your team, because of your relationship with them, will likely feel better if the information also comes from you. Therefore, you can summarize and highlight a few items from the daily updates and send it to your team at the end or beginning of the week. It will reinforce the message and it will reassure your team.
· Stay Flexible. During challenging times, individuals are more likely to only communicate based on their style. Therefore, keep in mind that some team members need reassurance and repetition, while others function well with just enough information. Although you do not have to adjust to everyone’s style, it is important to notice those who seem to need more from you, and circle back with them as you are able.
· Capitalize on Technology. Notice who in your team is more tech-savvy and encourage them to find ways to enhance connection amongst the team members. The current situation is giving everyone an opportunity to explore new ways to connect and communicate with one another. Therefore, you and your team might institute a new way of communication that will make the practice flow more effective after operations return to a sense of normalcy
-
Compassion Fatigue +
Compassion fatigue refers to the feeling of exhaustion that can be experienced by health care workers, both clinical and non-clinical. This feeling is not just physical – though this is a large component – but it is also mental and emotional. No one is immune to this; in fact, one should expect it as the current COVID-19 situation continues to escalate. The amount of time, effort, energy, and even sacrifice, will begin to take a gradual toll on you.
It is important to remember that everyone is impacted differently and at different times. Some managers might experience it during the situation while others will experience it once it plateaus and they no longer feel “on stage.” Regardless of when or how you experience it, please know that the experience is valid, and the recovery period is vital. This recovery period does not have to be postponed until it is over. There are a few things you can do to build-in recovery periods and mitigate how you and your managers are being impacted:
· Take Time to Eat. It can be tempting to just “grab-and-go” but even if you only take 10 minutes, sit down and put away your phone. Notice the meal in front of you and try to enjoy it. Consider those 10 minutes as “sacred” and avoid distractions or even conversations about the current situation. This will give your mind a “mental break” from everything.
· Set Appropriate Boundaries. Understand your own physical and mental limitations and honor them by pacing yourself and avoiding over-commitment. It’s ok to say no when doing something could potentially be more harmful because of your own physical and mental health.
· Be Mindful of Energy Changes. Everyone’s energy fluctuates during the day, or even during the week, so be mindful of when you seem to have the most as well as when you tend to run low. This information could help you in how you structure your schedule or how you approach tasks.
-
Courage +
Our news outlets are reporting daily on the brave and heroic efforts of our health care workers, our first responders and our everyday community members sharing and showing acts of kindness, compassion and courage. Courage is the ability to do something that frightens us. Physical courage is bravery in the face of pain or grief. We normally think of courage as a trait or virtue. But courage can also be thought of as a behavior. Physicians demonstrate this behavior of courage throughout their practice of treating patients. The risks to physicians such as physical or mental harm, burnout, second victim syndrome or contacting a virus has been present for quite some time in American medicine. So, what is different now that we are amid a pandemic. The difference is that these behaviors of courage no longer are hidden. The media, social networks, and added communication forums have uncovered something that those in healthcare have always known, nearly never talked about and most likely just assumed. This is not a time that you see physicians standing up and speaking about courage. They are putting into action those qualities of courage as they always have. This brings us to moral courage, the ability to act rightly in the face of popular opposition, shame, scandal or discouragement. Morale courage involves deliberate or careful thought. Moral courage is the courage to act for moral reasons despite the risk of adverse consequences. What we are seeing all around us; in hospitals, outpatient clinics, makeshift tents, shelters is the morale courage of those men and women who took an oath. An oath that is held sacred by physicians to treat the ill to the best of their abilities. This kind of courage is selfless, intentional, difficult and sometimes painful. Recently, when asked of a critical care physician treating COVID – 19 patients, why he takes the risk to himself and his family, he replied, ‘that’s just what we do’
-
Dealing with Uncertainty +
Situations where information is constantly being updated and disseminated through various means can generate response related to a sense of uncertainty. Although it might seem like access to information can help mitigate this, it actually generates the opposite. Individuals become flooded and this leads to confusion, misinformation, and even a sense of mistrust. Therefore, it is helpful to keep things in perspective and manage the sources and amount of information being considered. At the same time, uncertain situations are training grounds to practice flexibility and re-organization of resources.
Being under an atmosphere of uncertainty often makes it harder to make decisions because of fear. This leads to added pressure and a cycle of second-guessing that could hinder your ability to do your best. Here are a few strategies you can try:
· Know the Facts. Myths and misinformation abound and they can become like a virus that spreads through social media and conversations. Staying vigilant and well-informed reduces the sense of uncertainty; even knowing that we do not know can be more helpful than filling in the gaps with suppositions.
· Reflect on Past Successes. Uncertainty can magnify worse-case-scenarios and make them more likely in our mind. Reflecting on past successes can give you a different perspective about your ability to face challenges.
· Focus on What Matters. As the information continues to flow and protocols change, remain focused on what is most important and what the ultimate goal is. This will help in making more informed choices and minimize unnecessary pressure or distractions.
-
Developing Winning Habits +
The current crisis has made it challenging for anyone to rely on previous habits to accomplish their day-to-day goals, much less long-term goals.
Due to the ever-changing nature of the situation, it seems like individauls have given up on creating routines and habits because they assume that they might not be able to engage in them because of the need to react. Although, there is an element of truth to these difficulties, habits are small steps that will accumulate over time and have a big impact.
It is important to develop, practice, and reinforce habits. Habits are practices that become second nature – like driving or brushing your teeth – and free up time, energy, and effort to engage in other practices. Here are a few strategies to help you:
· Change the Approach. Often, individuals approach a goal by focusing on what they want to accomplish (the goals), and then developing a system (method) to reach it. The problem with this old method is that crises often derail or interfere with the method, causing frustration and even discouragement. Instead, change the question from “how do I reach this goal?” To “what type of person would want this goal and what would s/he do today under these circumstances?” Although both questions seem similar, there is a vast different. The second question aligns a goal with an identity and frames it within a self-efficacy attitude.
· Reinforce You Identity in Small Ways. Think of every action you take as a vote for the person you want to be. As you engage in small habits, you are “casting votes” towards the person you are becoming rather than relying on the old “fake it until you make it” approach.
· Scale it Down to 2 Minutes. Whatever your ultimate goal is, scale it down to one behavior you can accomplish in 2 minutes. If it is to exercise regularly, take a 2-minute walk; if it is to read one book a month, read one page; if it is to meditate once a day, download one app. The purpose is to begin to move towards your goal by making it easy to do. This works because you begin to develop a new routine (2 minutes at a time) before you improve it and add more to it.
· Don’t Wait to Start. Challenging situations have a tendency to create the illusion that this is not the right time to begin a new routine. However, it might be the best time to do so because of the uncertainties and the need to have more control over one aspect of your life. A small step – eating right during lunch, walking for 5 minutes, meditating for 1 minute, etc. – can make the difference when you focus more on the step than in the ultimate goal. Right now, going to the gym 5 days a week, going away for a weekend, etc. are not realistic but it does not mean you have to wait until the current situation ends to “get back to normal.”
-
Developing Your Team During Difficult Times +
During challenging times, teams like individuals, Are faced with choice to stay stagnant or develop a new way of performing. The bottom line does not change, which is taking care of patients; however, the methods might have to change due to the new problems and difficulties. These periods give leaders the opportunity to develop and improve their teams and create a stronger team.
It is important to note that this process is full of trials and errors because of the newness of the challenges. This is why finding ways to involve your team will maximize efforts while minimizing the burden of dealing with problems. Below are a few strategies that could help you, but please reach out to us with any specific need or question. At the Wellness & Resilience program, we strive to provide consultation to help leaders like you navigate challenges.
· Acknowledge the Problem(s). The first step to solving a problem is to acknowledge there is one and taking proactive steps to solving it. Usually crises create problems while revealing other ones. Notice what issues may hav been there for some time and take time to address it.
· Create a Way for Upward Communication. You can use informal times to ask for feedback, send out brief surveys to your team, or spend time at the end of meetings asking for their perspectives. Obtaining your team’s input regularly will ensure you are aware of issues that might be developing and take prompt action before they escalate.
· Break Down the Problem(s). It can be tempting to tackle a problem head-on with a solution that seems adequate. However, breaking down a problem will increase the chances of addressing any collateral issues that could sabotage the outcome.
· Lead with Questions. In developing teams, it is always best to ask questions rather than make assumptions about what they need. During difficult times, individuals may not be open to discussing their needs unless they are asked. Asking them also validates their experience and send the message that whatever solution is implemented, their concerns were taken into consideration.
-
Finding Balance in Uncertain Times +
The current COVID-19 situation has tipped the work-home balance toward work even more than before. It can be challenging to disconnect from work if you are going home because of the constant need to stay informed about the ever-changing situation. Furthermore, many providers are having to engage in practices and activities they never had, to ensure the safety of themselves and their loved ones. It has become increasingly more difficult to find and maintain an adequate work-home balance in the current situation.
· Disconnect as Much as Possible. Whenever you make it home, spend undivided time with your family. If they have questions about the current situation, have a “rule” to where only 10-15 minutes will be devoted to debriefing about it. After that, go for a walk, play games, watch movies, or do anything as a family that gives you a sense of normalcy.
· Enjoy a Relaxing Hobby. If you do not have a hobby, look up ideas on the internet and select one that appeals to you. It needs to be non-medicine related and where you can make mistakes or do not have to finish it. Examples can include gardening, cooking, organizing, writing, etc.
· Honor Your Own Needs. Although some individuals thrive off of socialization and interactions with others, others prefer solitude and time to themselves. Recognize your own and honor it by establishing boundaries.
· Have Fun. Find shows, movies, books, series, etc., that provide humor and distraction for you. Make an intentional decision to engage in this activity at least a few times a week. Including others – even remotely – will richly enhance the experience
-
How to Respond to What You Are Feeling +
In times of uncertainty and as challenges increase, it is expected that decision-makers will face criticism from different sources. Keep in mind that individuals often speak from their frame of reference and subjective experience. Therefore, there might be some validity in their perspective despite the presentation or lack of the full picture.
As a physician or advance practice provider, you might find yourself in the middle where you receive guidance and expectations from senior leadership while providing this to your team. This places you in a unique position to influence while being influenced yourself. Managing this middle ground can be challenging and create a reputation that will follow you after the crisis has passed. Here are a few strategies that can help you with the concept of criticism:
· Remain Open. Although as a leader you are providing directives and disseminating information that is coming from your own leaders, remaining open and flexible to new protocols. You set the tone and can create an atmosphere that is inviting to adaptation and evolution.
· Avoid Criticizing. It can be tempting to speak your mind and share your opinions with others. However, it can backfire because it erodes the trust your team has in the organization as well as the way you might be perceived. Discussions are different than criticism. A criticism is a conversation with someone who is not involved in the problem nor in the solution.
· Wait to Respond. If you are on the receiving end of criticism, give yourself a few hours to think through the criticism and recognize the value in it. During the current situation, individuals’ sensitivities are heightened so taking some time before responding – if it’s necessary – can be more helpful.
· Stay Focused on the Goal. Facing criticism can be discouraging and add more pressure; however, successful physicians, athletes, and business individuals have in common their commitment, determination, and passion to achieve a goal. The method, and even the timing, might change but their vision and mission remain in front of them. Stay focus!
· Reach out to Mentors. As a leader, you are in the frontlines of the current situation. Therefore, you will be the first one to face criticism from others. Reach out to mentors and/or professional coaches who can provide you with perspectives, strategies, and the support you need to keep going.
-
What steps can I take to improve my resiliency? +
The current situation, although at a global scale, is similar to what many individuals, families, and even communities often faced during a tragedy. They are deeply impacted because of the sense of loss. As a result of COVID-19, many have and will continue to lose their lives; many have lost their jobs; many have lost their sense of community due to social distancing; and many have lost a sense of safety because they do not feel comfortable being outside due to the potential of contracting the virus. All of these losses are experienced deeply by everyone, and depending on previous losses, they can be magnified in physicians and advance practice providers due to their being in the frontlines.
Acknowledging that everyone is and will experience these circumstances differently, here are a few general strategies:
·Dispel the Misconception of Grief Stages. Unfortunately, many have been taught the Kubler-Ross model of grief as “stages.” However, the author never intended for them to be taught in a sequence manner because these are types of normal responses in no specific order. Therefore, it is common for you to experience one or all of them at the same time for short periods of times. Think of your responses like an ocean wave that comes, peaks, and then washes over.
· Be Open to Your Own Experience. Negating or neglecting your experience will eventually lead to burnout. Acknowledging and finding meaning to your experience can be helpful during these times. Rely on your culture, religious beliefs, and/or values to help you face your experiences.
· Move from Why’s to What’s. During times of loss, it is very common to ask why questions. Individuals want to understand with the hope of making sense of the loss and be better prepared for the future. It is more helpful to ask what can be done and what is within your power and control.
·Express Yourself. Understand that not everyone benefits from talking to someone; however, everyone benefits from expressing their emotions. This means that you might do it through journaling, painting, blogging, or spending time with someone who understand you even, or especially, if you are not able to find the words to express yourself.
Please let the Wellness & Resilience Program be of support to you during these times and provide you with more personal strategies that will fit your needs.
You can reach out to Mary Senne, PhD at 407-718-1091 or Kenny Tello, LCSW at 407-430-7540
-
Leading Through Difficult Situations +
Leadership is not a matter of position but a matter of influence. Difficult and challenging situations often reveal traits in people that can help them establish more influence around them. It is not uncommon for individuals to respond differently during difficult situations and transitions. There are those who get caught up in the details and expect to be told what to do. And there are others who look at the big picture and take charge of the decisions that need to be made. This is not just a dynamic at the highest levels of the organization. In fact, leading is an attitude that can be fostered and enhanced by anyone regardless of role, title, and even experience.
Here are some strategies to enhance your leadership:
· Be Mindful of Your Presence. Leaders are naturally looked to for information, reassurance and guidance. Therefore, it is important to keep this in mind as you go into a room, get on a call, or carry conversations with others.
· Think Outside the Box. During difficult situations, be creative and innovative while following essential protocols. Leaders do not act alone; in fact, they often do their best thinking while discussing ideas with others so speak up and share your ideas.
· Recognize Limitations. Leaders often have a tendency to keep going and expect the same amount of output from others. However, everyone has a different threshold and abilities. Being mindful of others’ limitations can make it easier to lead them, while saving you from unnecessary frustrations.
· Stay Open to Feedback. As a leader, staying open to others’ ideas and feedback demonstrate respect and humility. It will enhance trust, engagement, and commitment from those around you who are doing the best they can with what they have.
-
Managing a Sense of Powerlessness +
Critical situations such as pandemics can instill a sense of powerlessness and create an aura of limited options. Although the current situation is certainly exerting pressure and restricting resources, it is also true that there are numerous ways in which this situation is being managed effectively. Therefore, it is important to keep an adequate perspective and make a conscious effort to:
· Avoid Asking “why.” Why questions compel people to look for reasons; however, in times of increased uncertainties, this search can make matters worse. Instead, ask how and/or what can be done about a situation. How and What questions help generate solutions and move conversations toward resolutions.
· Change Your Focus. Notice and focus on what you can do more than on what you wish you could do. Focusing on your abilities, talents, and how you are able to use your skills will give you a sense of empowerment.
· Read or Watch Inspiring Stories. Books such as “Man in Search of Meaning” by Viktor Frank, or documentaries such as “I am” on the life of Tom Shadyac, can be sources of great comfort and perspective. Share other books, movies, or documentaries with those around you so people have alternatives to the news and social media.
· Increase Self-Efficacy. This concept is related to the belief in one’s own abilities and capacities to influence or accomplish a goal. It is largely influenced by perceptions and attributions. Therefore, listen to others’ feedback, especially from those you admire and respect; and remember the times you have effectively dealt with difficult situations.
Increasing a sense of empowerment and self-efficacy provides the “grit” and drive needed to keep going in moments that are full of uncertainties.
-
Managing the Pressure +
The role of a physician or advance practice provider is full of task, requirements, and responsibilities well beyond patient interactions. These responsibilities add to the pressure of maintaining an optimal level of performance. Providers around the world are facing an unprecedented situation that is forcing them to remain vigilant of their own energy, time, and resources. Here are a few strategies to help you:
· Pick Your Battles. In times of limited energy, time, and even resources, it is best to be intentionally selective on what conflicts, negotiations, and even arguments you engage in to minimize frustrations and a sense of apathy.
· Check-in with Yourself. In the midst of everything that is asked of you, it can be easy to lose track of your own needs. Use your phone or smart watch (if you have one) to schedule 1-2-minute blocks of time during the day to take a step back and notice where you are in regard to your energy.
· Delegate Responsibilities. Providers are notoriously hard workers who strive to provide best and optimal care to others all of the time. Although there are responsibilities and functions only you can do, there might be other ones that you could delegate to individuals in your team that are trustworthy and resourceful.
· Use Your Resources. Take advantage of Orlando Health’s resources such as wellness coaches, provider liaisons, and other individuals to help you manage the ever-growing amount of responsibilities.
-
Perceived Social Isolation +
Nearly 1 in 5 Americans 65 and older are socially isolated, according to AARP Foundation. Research finds that this public health epidemic affects more than 8 million age 50-plus adults and is growing as 10,000 Americans a day turn 65.
As we watch social distancing behaviors transform our workplace and our communities, we may begin to feel socially isolated, withdrawn or even lonely. Loneliness reflects a temporary lack of contact with others. Social isolation is the complete or nearly complete lack of contact between an individual and society. Perceived social isolation (PSI) is the experience of perceiving oneself as isolated. PSI is a risk factor for and may contribute to a person’s poor overall cognitive performance, poor executive functioning, cognitive decline and even their heightened sensibility to threats.
Even if we are not by definition, isolated from others, we may perceive that we are emotionally/psychologically isolated. Social interactions of individuals who are perceiving a sense of social isolation may tend to be more negative and less satisfying overall. This can potentially impact relationships if we are not mindful.
So, what can we do to stay connected to each other and at the same time stay safe?
1. Use the technology at hand: phone call, text, FaceTime,
2. Join a virtual group such as exercise, yoga, meditation, chess
3. Take a 10-minute walk during your workday, see others & greet others
4. Set aside time to call old friends, colleagues, mentors
5. If you have a face to face conversation (6 feet apart) Be present, me mindful
-
Can Perseverance and Anxiety Co-exist? +
Perseverance is persistence in doing something despite difficulty or delay in achieving success. When you search for synonyms for this definition you find words like tenacity, determination, resolve, drive and diligence. These are descriptions so readily associated with physicians. As the co-director of the physician wellness & resilience program for Orlando Health medical staff I have had the privilege to work with countless physicians who demonstrate these qualities, often to the detriment of their own well-being. Physicians are often self-reliant, and many do not ask for help. This trait may not serve them well during this time of increased uncertainty, increase workload, additional anxiety about family safety and what the future of medicine will look like. Communicating ones’ fears and anxieties to someone else can help reduce these uncomfortable feelings.
A recent article in the Journal of the American Medical Association (2020) written by Shanafelt, T., Trockel, M. of Stanford School of Medicine and Ripp, J. of Icahan School of Medicine at Mount Sanai, New York, NY report their findings as it relates to understanding the sources of anxiety among physicians, residents, fellows, nurses and advanced practice clinicians. During the first week of the COVID-19 pandemic the investigators explored three key concerns. They looked at what clinicians were most concerned about, what clinicians needed from their leaders and what sources of support they believed would be most helpful. The concerns expressed centered around access to appropriate PPE, exposure to COVID-19 at work and taking the infection home, not having rapid testing, uncertainty that their health institute would support their personal and family needs including child care and lack of access to up to date information.
Sources of anxiety for any physician can vary when you consider individual circumstances, degree of healthy coping strategies and available social supports. However, it is helpful to recognize that these anxieties are shared, they are to be expected and that you are not alone.
A key to coping is to label the anxiety, recognize the symptoms, communicate with a trusted colleague or friend, a wellness coach and if need be, consult a mental health professional.
-
Positive Psychology Strategies to Deal with COVID-19 +
Many physicians are being asked to support the well-being of others. In times of great stress and uncertainty, drawing on the principles of positive psychology and coaching can be helpful. Kerri Palamara, MD, FACP, Director of the Center for Physician Well-being at Massachusetts General Hospital and Physician Coaching Services Lead for American College of Physicians presents positive psychology strategies to use in a time of crisis.
Deep Breaths: Everything going on can feel overwhelming, pausing to take slow deep breaths can help.
Offer gratitude to a colleague: Provide authentic praise for a job well done or positive feedback – this strengthens connections between physicians, sparks motivations in both individuals, and boosts happiness.
3 Good Things: Rather than scrolling through the news or thinking about what was challenging that day spend a few moments jotting down 3 good things that happened to you that day
Share a good story: Physicians often don’t share good stories with colleagues. Sharing positive stories connects us to those we are talking to and boosts happiness, creativity, and open-mindedness
Reach out and talk to someone: The next time you are busy or overwhelmed at work, consider talking to someone about something non-medical for just a few moments, rather than burying yourself further in your work. Use Zoom or Facetime
Try laughing – at yourself or something funny. Laughter is contagious, and data shows that even if it is not authentic, it still makes you feel better by improving coping, resiliency, and health
Put one foot in front of the other. When you are really overwhelmed, focus on the baby steps and ask yourself, “what is the next thing I need to do?”
-
Resilience in Critical Times +
Resilience has been defined as “the ability to bounce back.” Although this is true, resilience is more than that, and it is closely related to the concept of thriving. Thriving speaks of the ability to adjust and adapt to the current situation without being consumed by it. In fact, adaptability has been shown to be a key component of individuals who endure and face unprecedented experiences and do so effectively. Therefore, to be resilient is to be adaptable.
As incoming information increases and the calls, consults, questions, demands for your attention, etc., increase, it can be challenging to find an adequate way to adapt and remain flexible. Although challenging, being more intentional about the approach can aid in the development of personal and professional resilience. Here are a few ways to do that:
· Do Not Expect Perfection. Other than ensuring optimal patient care, give yourself room to miss some emails, running late to a meeting, or forgetting to text someone back. Remember that you are doing your best and right now, that is more than enough.
· Spend Time with “Builders.” Everyone responds differently during critical situations. Therefore, avoid those who seem to be caught up in generating drama or who seem to complain excessively. Instead, spend more time with those colleagues who provide input, feedback, and information that lifts you up.
· Remain Purpose-Driven. Adaptability does not mean changing your goal but changing your methods. Continue to maintain your sight on your purpose while being open to alternative or innovative ways of achieving it.
During challenging situations, it is inevitable that there is a part in everyone that will change. Remaining resilient and adaptable will increase your ability to thrive and develop into a better person and provider all around.
-
Responding to the Levels of Concern +
Healthcare organizations throughout the world are feeling the impact of the current situation. In many respects, the impact is multi-faceted and difficult to predict. This has generated several responses and problems in providers and team members alike. Some providers are concern about their sense of safety, while others are concerned about their own physical and mental health. Some providers are worried about their team members while others are worried about the organization. It is safe to say that everyone is concerned about different aspects of the current situation. Therefore, there are a few strategies that you can use with your teams:
· Improve Attitude. Emotional and mental health are rapidly deteriorating in the face of the current situation. Encourage your team to take care of themselves and to take advantage of resources available to them, while modeling that attitude and behavior yourself.
· Create Weekly Huddles. If you have not done this, develop weekly huddles with your teams where they have a chance to express concerns, ask questions, and hear information firsthand. Although the organization is sending daily emails, hearing from you will reinforce the message. These huddles with your team can provide a sense of community during the social distancing. Keep it somewhat informal so everyone can feel more relaxed.
· Enhance Their View. Aa a provider, you are a leader, even if you do not see yourself as one or do not have a specific title. The way you are viewed, the narratives others are developing of you will remain months, even years after we work through COVID-19. Therefore, during this time, spend time thinking about how others might be perceiving you, how you need to show up, and how you are impacting someone else’s feelings.
· Communicate Empathetically. Before providing your opinion or a solution, acknowledge what the other is feeling. Acknowledging the difficulties and uncertainties and how they might be impacted. This lets them know you care and opens them up to hear you without misunderstanding you or becoming defensive. This is a time of heightened sensitivity and empathy can make a difference in the communication process.
· Speak Directly to Their Fears. Many team members and even colleagues might reach out to you about their own stress and fears. Avoid giving them ambiguous answer. If you do not have the answer, say so. If you know the answer and it is ok for you to share it, say it. Individuals can bounce back easier from bad news than uncertainties.
-
Six Ways to Cope with Your COVID-19 Grief +
Every time we experience a loss — a job, a loved one, even a sense of normalcy — we will also experience a type of grief. COVID-19 has caused many of us to experience different types of losses, especially because we know life will not be the same when it is over. There is a lot of uncertainty and this could delay our ability to cope and work through these losses. However, the current situation can be seen as a sort of bootcamp for life post COVID-19, where the choices you make now will make a huge impact on your long-term goals, and more importantly, who you are becoming in the middle of this pandemic.
Here are six strategies to help you manage your experience, and even some of your losses:
First, value your emotions. There are five common responses (not stages) to losses: denial, anger, bargaining, depression, and acceptance. Grief is not a linear experience and these responses can occur at any time, often in combination with other emotions. Try looking at grief as a package, where you will find several things in it but each has value in moving you through the experience.
Second, own your experience. It is important to remember that your experience is unique. Many of us are home now and routines have changed drastically. I’m sure many of you are probably grateful to spend added time with your family, while some others are feeling added pressure and stress. Social distancing has created a sense of isolation that has magnified any issues in the family, the couple, and the individual. Make a routine with behaviors that will only take you 2-5 minutes to accomplish. As you engage in these new habits, they will progressively move you in the right direction. This will help you have a different experience and even improve what was already there.
Third, ask the right questions. Whenever we experience losses and enter a sense of uncertainty, it is very normal to ask “why” questions: Why did this happen? Why now? These questions are common because in the middle of uncertainty we want to make sense of the situation and figure out what to do. Therefore, questions that lead to answers and actions can be more helpful. Questions such as: What can I do while this passes? What is one area I can improve on with my extra time? How can I connect with my loved ones better? These questions will empower you and help you move through your grief more adequately.
Fourth, express yourself. Expressing what you are going through will unburden you from how the grief and sense of loss might be accumulating in you. Unfortunately we are seeing an increase in family problems and it is partly due to how individuals are choosing to express their emotions. Therefore, find a way to express yourself such as talking to someone, journaling, playing an instrument, listening to your favorite music, painting, going for a walk, prayer, gardening, etc.
Fifth, strive for growth. As human beings, we have a need to have purpose and grow. During COVID-19, many feel like they have lost this because they are “stuck at home.” However, we actually have an opportunity to re-define what gives us purpose and what is helping us grow. Begin each day with 2 specific goals you want to accomplish that day. This could be just changing out of your pajamas or finally reading for a few minutes. The goals do not have to be big and complicated; in fact, make them so easy to accomplish that you will not need a lot of motivation to get you started. Track these goals and at the end of each day, you will have a sense of accomplishment that will compound at the end of the week. Think of your daily plan as an investment into the person you will be post COVID-19.
Sixth, create significance. Our minds like stories and giving meaning to situations. Whatever meaning you are giving to this pandemic will highly influence your responses and the actions you take. For instance, if COVID-19 means death, stress, losses, the government’s way of controlling us (yes, there are several people out there who believe this), then you will feel a sense of dread, powerlessness, depression, and frustration. Instead, give this situation a different meaning such as reset period, growth catalyst, opportunity to redefine priorities, and/or a chance to invest in your spiritual beliefs.
Use these strategies to help move through this sense of loss and grief all of us are experiencing collectively. We’re not immune to what is happening, but we can make the most of this time. We can either focus on what we have lost, or focus on what we have left. “If you want to change the world, go home and love your family.” Mother Teresa
-
Spiritual Health +
In a recent article published in Medscape, April 13, author Elizabeth J. Berger writes about the necessity for health care workers to not ignore their spiritual health. Spirituality is defined as “the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred. " As a chaplain of a large health institution she argues that connectedness, meaning and purpose are essential human needs, especially for health care workers during the COVID-19 crisis. However, it has been my experience coaching physicians that the same drive for connectedness can also have negative consequences including emotional exhaustion, depersonalization and even depression. So where can spiritual health fit in the overall goal of reducing stress, reducing empathy fatigue and increasing a sense of well-being. One answer may lie in how one expresses meaning and purpose. With the physicians/patient relationship, compassion is the expression. Compassion is the act of showing concern for the sufferings or misfortunes of others. If someone shows kindness and a willingness to help others, they are showing compassion. When you have compassion, you are putting yourself in someone else’s shoes and really feeling for them. The acts of compassion you share help define your purpose and the meaning of your work. Hence the notion of spiritual health. It is when you the physician, health care worker is unable, or it becomes difficult to separate or withdraw from that human interaction on an emotional level that one begins to experience depletion. One strategy to avoid or minimize the likelihood of depletion is to be mindful. Example: after each patient encounter pause for one minute, take a conscious breath, identify what you are feeling, label it, allow it to be felt fully and then move on. This step allows for resilience building.
-
Wellness in Challenging Time +
It is common for providers to be other-focused. It’s just the nature of your job and the commitment you have made, to take care of others. However, this often comes at a cost to your own wellbeing.
Challenging times, like the ones we are currently facing, is taking a toll on providers’ wellbeing because of the increasing demands and seemingly limited resources. It is important to realize that wellness is not the result of hours engaging in an activity, or days away from your job. In fact, research has shown that small changes can increase your wellbeing much more than a long vacation or having hours to yourself. Vacation and extended times to do what you enjoy are certainly important, but because of the nature of your job and how infrequent these periods might be, they are not the best sources of wellness.
Wellness begins with a decision to make it a priority. It also begins by recognizing that we have different areas and while we might be doing well in one area, the key is to take care of the other areas to have additional reserves during challenging times.
· Physical Area: Exercising, eating properly, and having enough sleep are the top strategies. You can also stretch, get up every hour or two and take a 5 minute walk, avoid relying on energy drinks to get/keep going, and be mindful of the nutritional value of what you eat as some food will make you feel more tired.
· Mental Area: Stay curious about your profession, reach out to a mentor or someone you respect and catch up, read for pleasure, and listen to podcasts while you drive.
· Emotional Area: Smile, engage in conversations with individuals who lift you up, recognize your emotional threshold, and keep it simple.
· Spiritual Area: Spend time practicing your spiritual beliefs, recognize your place and role in the lives of others, and look for a deeper meaning in the current circumstances
Critical Incident Response
Critical incidents are never scheduled and medical providers seem to “just keep going” during and after the incident is over. Coaching can be a tool to use during and after the critical incidents to prevent and/or ameliorate any impact on the providers and their teams.
Physician coach Kenny, has developed a protocol on how to support team members after a critical incident. A critical incident is defined as an event that has a stressful impact sufficient enough to overwhelm the usually effective coping skills of an individual. In other words, it is an experience that has the potential to make it difficult for the individual to be able to do his or her job without being bothered by overwhelming thoughts, emotions, and body sensations. Examples of critical incidents could include suicides, loss of patients, and man-made disasters such as bombings, significant shootings, and assaults.
These critical incidents are almost always unexpected and by their very nature, they can be overwhelming and create a sense of confusion, powerlessness, and at times even hopelessness. A physician coach is trained to help medical staff through these experiences and provide referrals to other professionals if deemed appropriate and necessary.
If you’re in crisis, please call the National Suicide Prevention Lifeline at 1.800.273.TALK (8255) or contact the Crisis Text Line by texting TALK to 741741.If you have Orlando Health Team Member Insurance (Health Choice) you can contact Orlando Behavioral Healthcare at 407.637.8075.
Types of Stress
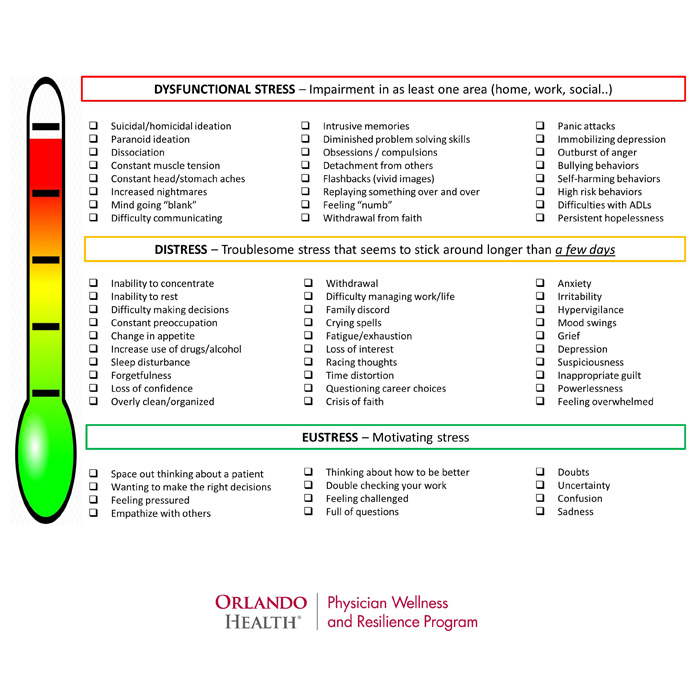
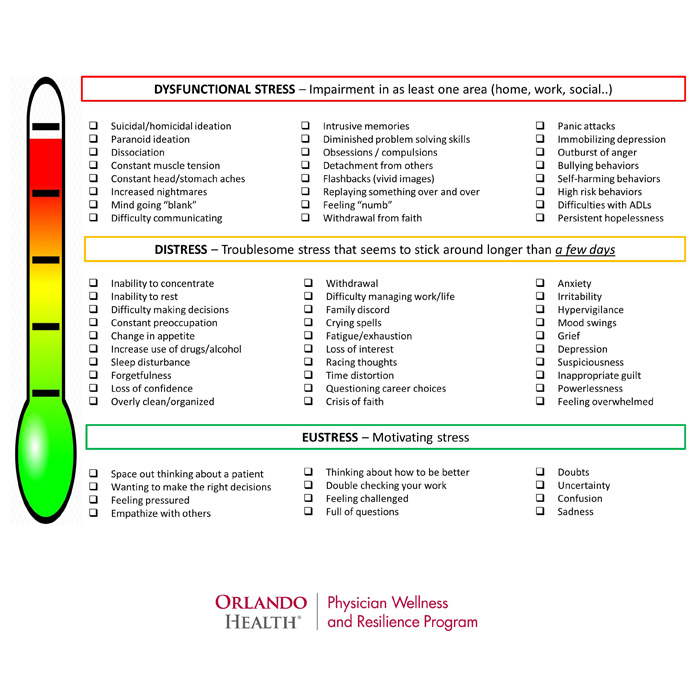
It is common to have a myriad of responses following a critical incident. Everyone is different and therefore, everyone is impacted differently. It is important to do a “checkup” periodically to ensure your responses are not developing into unhealthy and even dysfunctional responses. Please use the following “wellness thermometer” to check where you are and contact us with any questions.

ER Wait Times
Information will update every 5 minutes. ER Wait Times are approximate and provided for informational purposes only. Estimated Wait Times as of: Monday, September 15, 2025 3:35 AM
|
|
Wait Time | |
|---|---|---|
| Orlando Health - Health Central Hospital | Directions | 3 min |
| Orlando Health Arnold Palmer Hospital for Children | Directions | 21 min |
| Orlando Health Bayfront Hospital Emergency Room | Directions | 1 min |
| Orlando Health Dr. P. Phillips Hospital | Directions | 6 min |
| Orlando Health Emergency Room - Blue Cedar | Directions | 1 min |
| Orlando Health Emergency Room - Crossroads | Directions | 0 min |
| Orlando Health Emergency Room - Four Corners | Directions | 2 min |
| Orlando Health Emergency Room - Lake Mary | Directions | 20 min |
| Orlando Health Emergency Room - Longwood | Directions | 5 min |
| Orlando Health Emergency Room - Osceola | Directions | 0 min |
| Orlando Health Emergency Room - Pinellas Park | Directions | 0 min |
| Orlando Health Emergency Room - Randal Park | Directions | 0 min |
| Orlando Health Emergency Room - Reunion Village | Directions | 0 min |
| Orlando Health Emergency Room - Waterford Lakes | Directions | 0 min |
| Orlando Health Horizon West Hospital | Directions | 0 min |
| Orlando Health Melbourne Hospital | Directions | 0 min |
| Orlando Health Orlando Regional Medical Center | Directions | 60 min |
| Orlando Health Sebastian River Hospital | Directions | 0 min |
| Orlando Health South Lake Hospital | Directions | 8 min |
| Orlando Health St. Cloud Hospital | Directions | 7 min |
