Survey Finds Most Americans Believe Pain and Urinary Leakage is Normal for Women After Having Children
Experts stress that pelvic floor damage is usually treatable without surgery and that women don’t have to live with uncomfortable symptoms
Orlando, FL (July 15, 2024) – A new national survey by Orlando Health Advanced Rehabilitation Institute finds most Americans believe it’s normal for women to experience pain, pressure and incontinence after having children. But experts say these are actually signs of pelvic floor issues, and while they are extremely common, affecting about a third of women, they are not normal.
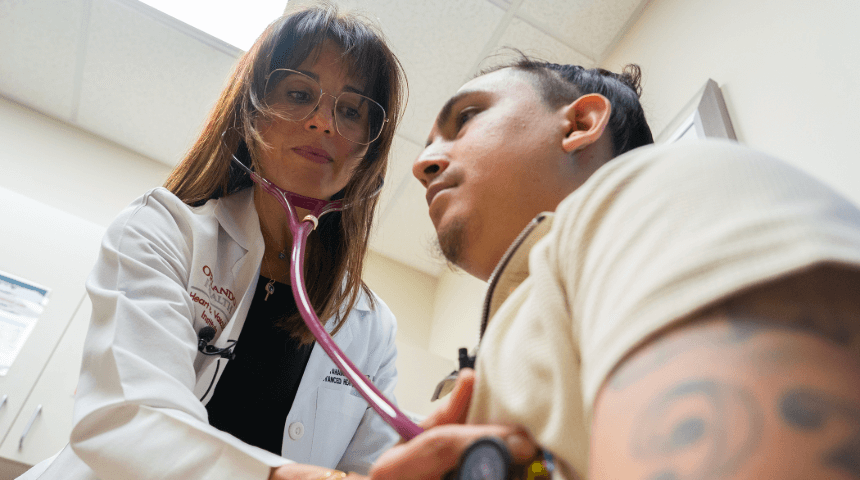
“When we say it's not normal, what we mean is it's not something you should have to live with. It's something you can rehabilitate and improve,” said Tessa Ladd, OTR/L, an occupational therapist at Orlando Health who specializes in treating pelvic floor dysfunction. “By strengthening and coordinating pelvic floor muscles and learning how to breathe and move in a way that supports the pelvic floor, these symptoms that so many women live with for years can be drastically improved.”

The survey, conducted by Ipsos, found that 71% of Americans believe it’s normal for women to have some urinary leakage after having kids, and more than half (51%) say it’s normal for women to experience pain during sex after they’ve recovered from childbirth — both telltale signs of pelvic floor damage.
The pelvic floor is the group of muscles and ligaments that act as a “hammock” to support the vagina, uterus, bladder and rectum. When they become damaged — most commonly brought on by pregnancy, childbirth or aging — they can cause incontinence, as well as pain and pressure that occurs when these organs slip from their normal position, known as prolapse.
“Childbirth puts a lot of trauma on the body, but just like with any other injury, muscles and tissues should have the ability to recover and support the internal organs,” Ladd said. “If that doesn’t happen, we can step in and help. The muscles within the pelvic floor are skeletal muscles. They’re something that we do have control over, just like our biceps or our calves, and we have the ability to strengthen, lengthen and relax them.”
The survey also found that 71% of respondents believe women should start working out to strengthen their abs and pelvic floor as soon after childbirth as possible, something Ladd warns can be counterproductive, as women feel societal pressure to “bounce back” after having a baby.
“You can begin to do some deep breathing and learn correct body mechanics in that early postpartum phase, but it’s also important to allow your body time to heal and not to do too much too fast,” Ladd said.
About a month after having her second child, Nicole Gerardi-Lukens suddenly felt immense pressure in her pelvis and went to the hospital. After being diagnosed with bladder prolapse, she worried she would need surgery and a lengthy recovery with a four-year-old and a newborn at home.
“I was so relieved when I was referred to a pelvic floor therapist,” Gerardi-Lukens said. “Tessa taught me things like how to breathe when I pick things up, and it made me realize how much pressure I was putting on my pelvic floor with everyday tasks. I didn’t always notice how much of that pressure I was feeling until I learned how to relieve it and could really feel the difference.”
After working with Ladd, Gerardi-Lukens can lift her child without the fear of pain or leakage and says pelvic floor therapy is something she wishes she had known about sooner.
“You know your body, and you know when something’s not right,” Gerardi-Lukens said. “As moms, we so often put everyone else first and even laugh off things like leakage as just a part of motherhood. But you have to decide if these are things you want to deal with forever. And if they’re not, seek the help of a pelvic floor therapist.”
Before women can get the medical help they need, they have to acknowledge the problem. Talking to your health care provider is the first step to finding solutions.
“If we have a problem with our knee, we could talk to anyone about it without shame, without feeling uncomfortable or weird about it,” Ladd said. “Everyone has pelvic floor muscles, yet it's something many women shy away from talking about, even with medical providers. When we open up about the symptoms we’re struggling with and understand that so many of us have this shared experience, we can help women live their lives free from pain and symptoms caused by these common and treatable issues.”
Survey Methodology
This survey was conducted online within the United States by Ipsos on the KnowledgePanel® from May 31 to June 2, 2024, and surveyed 1,020 U.S. adults ages 18 and older. This
poll is based on a nationally representative probability sample and has margin of sampling error of plus or minus 3.3 percentage points at the 95 percent confidence level, for results based on the entire sample of adults. For complete survey methodology, including weighting variables and subgroup sample sizes, please contact: [email protected].
About Orlando Health
Orlando Health, headquartered in Orlando, Florida, is a private, not-for-profit healthcare organization with
$9.6 billion of assets under management that serves the southeastern United States and Puerto Rico.
Founded more than 100 years ago, the healthcare system is recognized around the world for Central Florida’s only pediatric and adult Level I Trauma program as well as the only state-accredited Level II Adult Trauma Center in Pinellas County. It is the home of one of the nation’s largest neonatal intensive care units, one of the only systems in the southeast to offer open fetal surgery to repair the most severe forms of spina bifida, the site of an Olympic athlete training facility and operator of one of the largest and highest performing clinically integrated networks in the region. Orlando Health has pioneered life-changing medical research and its Graduate Medical Education program hosts more than 350 residents and fellows.
The 3,487-bed system includes 17 hospitals, 10 free-standing emergency rooms and nine Hospital Care at Home programs. An additional four hospitals and six free-standing emergency rooms are coming soon. The system also includes 10 specialty institutes, skilled nursing facilities, an in-patient behavioral health facility under the management of Acadia Healthcare, and more than 375 outpatient facilities that include physician clinics, imaging and laboratory services, wound care centers, home healthcare services in partnership with LHC Group, and urgent care centers in partnership with CareSpot Urgent Care. More than 4,950 physicians, representing more than 100 medical specialties and subspecialties have privileges across the Orlando Health system, which employs more than 29,000 team members and more than 1,500 physicians.
In FY 23, Orlando Health cared for 197,000 inpatients and 6.6 million outpatients. The healthcare system provided nearly $1.3 billion in total impact to the communities it serves in the form of community benefit programs and services, Medicare shortfalls, bad debt, community-building activities and capital investments in FY 22, the most recent period for which this information is available.
Additional information can be found at www.orlandohealth.com, or follow us on LinkedIn, Facebook, Instagram or X (formerly known as Twitter).