Off-the-Shelf Allograft Made with Live Cartilage Cells Streamlines Traumatic Joint Repair
An off-the-shelf, viable cartilage allograft offering a one-surgery solution is reshaping how sports medicine surgeons at Orlando Health Jewett Orthopedic Institute can treat traumatic cartilage injuries and focal chondral defects of the knee.
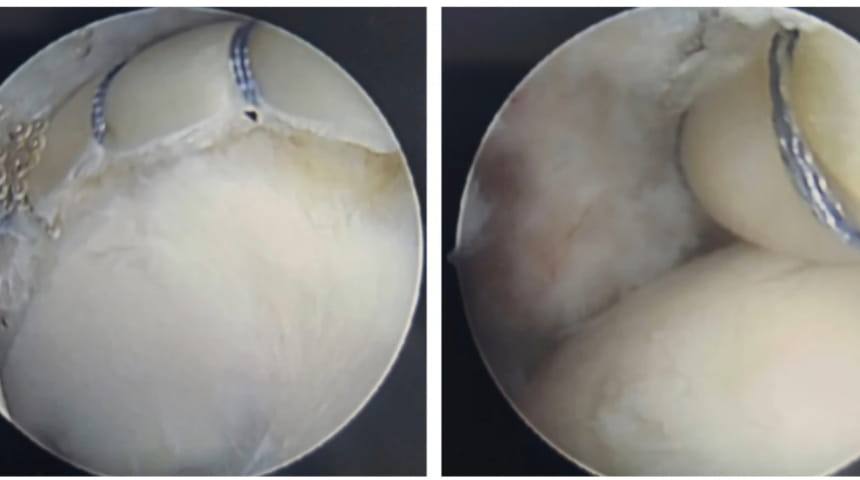
The novel product contains live, native chondrocytes with inherent growth factors combined in the operating room with an allograft lyophilized cartilage extracellular matrix. The resulting putty-like substance can be molded to fill a variety of cartilage voids without templates, trimming, sutures or glue. When activated and implanted, the chondrocytes migrate from the cartilage fibers and secrete components found in hyaline cartilage.

Unlike two-stage procedures such as autologous chondrocyte implantation (ACI) or osteochondral allograft (OCA) harvested from cadaver joints, the viable cartilage allograft molds to fit chondral defects in one surgical event.
“Matching the contour of someone's patella and trochlea with a cadaver bone can be technically challenging in the setting of osteochondral allograft transplantation,” says Abhishek Kannan, MD, a board-certified orthopedic sports medicine surgeon with Orlando Health Jewett Orthopedic Institute. “This product offers us an innovative joint preservation strategy for healthy patients with focal cartilage injuries and little-to-no arthritis.”
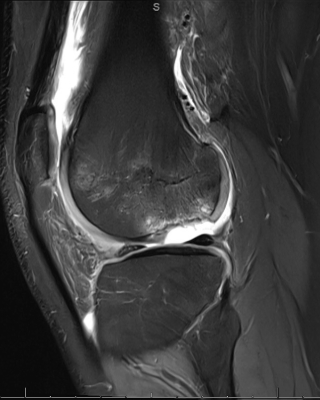
Dr. Kannan was the first surgeon in the region to use the cryopreserved product, choosing it as an option for a teenage patient with a traumatically displaced osteochondritis dissecans lesion. Initially, he planned a two-surgery standard of care — first to remove the large fragment (composed nearly entirely of cartilage), followed by ACI vs. OCA.
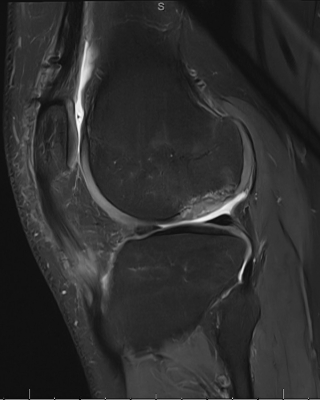
“We decided to try the live allograft first because, while we planned for two surgeries, we wondered if we could achieve something meaningful in a single-stage procedure under a single anesthesia event in a pediatric patient,” says Dr. Kannan. “Three months post-surgery, we obtained an MRI and noted the area we grafted healing beautifully — cartilage and underlying bone reconstituted, matching his femoral condyle contour perfectly. At three months, that’s remarkable.”
Dr. Kannan has since used the therapy to repair several knee joints, continually collecting and reviewing data. “It’s also been an option on the shelf when unexpected issues arise in the OR, like finding a focal cartilage defect during a meniscus repair surgery,” he says. “It appears to make surgical technique and workflow more efficient. It’s effective for the patient. That’s what we strive to find.”
The experts of Orlando Health Jewett Orthopedic Institute practice at Florida’s first and only orthopedic specialty hospital, which is a premier clinical destination for high-quality, multidisciplinary orthopedic care. Orlando Health is dedicated to revolutionizing patient care with outcomes advanced by specialists skilled in the most leading-edge technologies and involved in advanced clinical research and training.