Gynecologic oncologists at the Orlando Health Cancer Institute are using their advanced training and experience in specialized robotic-assisted surgery for innovative treatments of uterine and cervical cancers. Novel, minimally invasive surgical approaches to sentinel lymph node mapping and trachelectomy are helping enhance patients’ quality of life by avoiding lymphedema, reducing nerve damage post-operatively and conserving fertility.
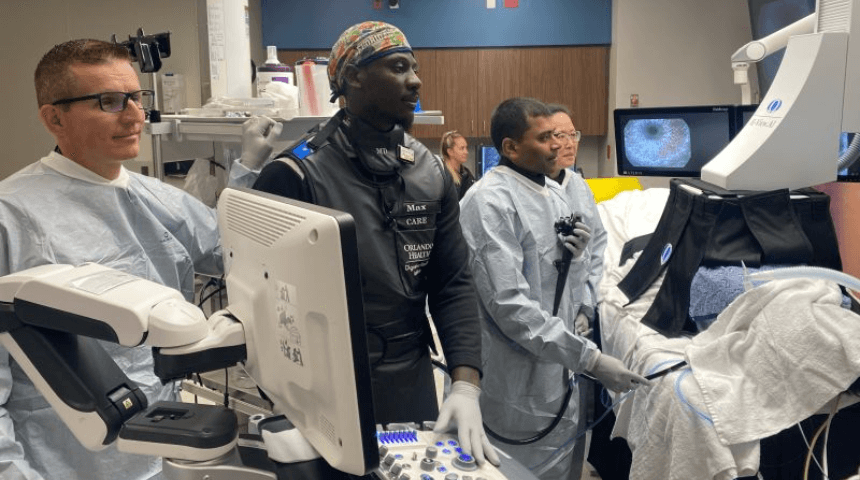
“We have developed targeted robotic protocols that can help enhance our cancer patients’ quality of life,” says Dr. Veronica Schimp, chief of Gynecologic Oncology at Orlando Health Cancer Institute. She was recognized in September for having completed more than 2,500 robotic surgery cases.
Mapping the high-risk sentinel lymph nodes adjacent to cancerous tumors is a standard diagnostic tool for breast cancer infiltration. Specialists at Orlando Health use the data from the Gynecologic Oncology Group phase III studies to best map nodes for uterine, cervical and even vulvar cancers.

Done robotically for increased accuracy, the procedure reduces the number of lymph nodes removed from 15-30 to four to eight, depending on the patient. “This is extremely helpful for those with higher-grade uterine cancers typically demanding a complete pelvic and periaortic lymphadenectomy,” says Dr. Schimp. “Less extensive dissection reduces lymphedemas and nerve damage, while lowering surgical risk.”
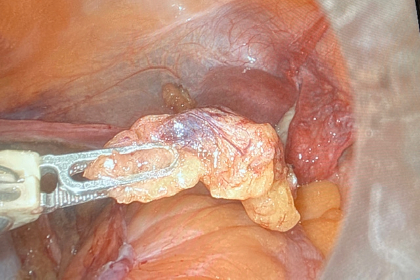
For women with small, localized cervical cancer, a radical trachelectomy offers a fertility-sparing surgical approach that removes the cervix, upper vagina and parametrium. The uterus is reattached to the vagina and a permanent cerclage is placed so the patient can hopefully carry her child to term. Women will need to have a cesarean section for their deliveries after this procedure as the cerclage prevents vaginal deliveries.
“Few specialists do these kinds of procedures, and we do enough of them to be very competent at them,” says Dr. Schimp. “It’s good when you can save a patient’s ability to have babies and take care of their cancers, too.
“We have had particularly good success doing robotic procedures for our patients,” she says. “Recovery commonly takes about two weeks, compared with four to six weeks for traditional open surgery.”
The Orlando Health Cancer Institute is accredited by the American College of Surgeons (ACoS) Commission on Cancer (CoC), the American Society of Clinical Oncology (“ASCO”) Quality Outpatient Practice Initiative (“QOPI”), the National Accreditation Program for Breast Centers (“NAPBC”), the American College of Radiation (“ACR”)/American Society of Radiation Oncology (“ASTRO”) and is among fewer than 50 programs in the nation recognized by the National Accreditation Program for Rectal Cancer (NAPRC) of the American College of Surgeons.