If you’re facing surgery for breast cancer, you probably have lots of questions, including what type of surgery, reconstruction options, what to expect during recovery and why you may be asked to consider genetic testing.
Here’s what you need to know.
- There are different types of breast cancer surgery.
- If you have mastectomy, you may not need radiation therapy.
- Breast reconstruction decisions and timing are up to you.
- Don’t expect a long (or maybe any) hospital stay.
- You will need to manage drains.
- Genetic testing could be valuable.
Surgeries fall into two general types. The first is a lumpectomy, where the goal is to remove the tumor while preserving as much of your breast as possible. This is often only an option when the tumor is less than 5 centimeters. The procedure removes the tumor and some surrounding tissue.
The second type of surgery is a mastectomy, which is the complete removal of breast tissue. There are variations of the surgery, which can be used to preserve skin tissue and/or the nipple, particularly when reconstruction will immediately follow the mastectomy.
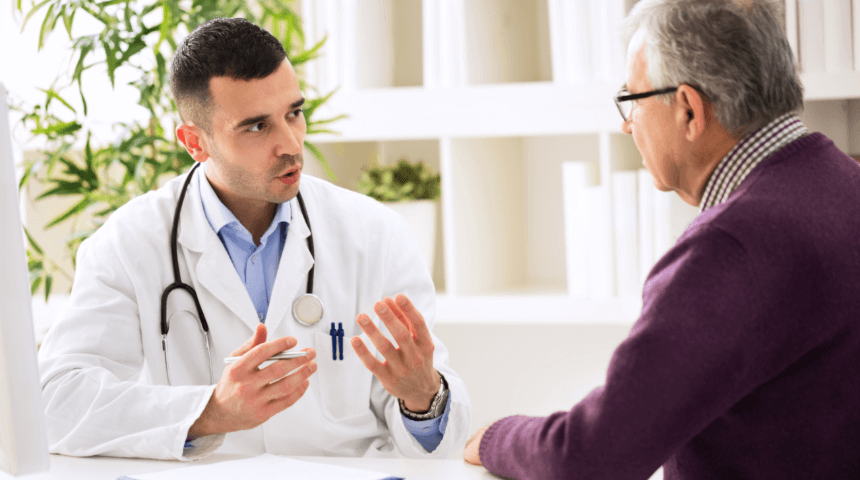
Your doctor may also recommend removing some lymph nodes from your armpit. This is called a sentinel lymph node biopsy. Your surgeon will perform a biopsy to check whether the cancer has spread beyond your breast.
If you have a lumpectomy, that will almost always be followed by a course of radiation therapy. This increases the odds that all the cancer cells have been destroyed and lowers your risk for a recurrence. But after a mastectomy, this treatment may not be necessary. Your doctor and care team will evaluate the tumor and other risk factors before making a recommendation to you.
After a mastectomy, you have several reconstruction options. Some women choose reconstructive breast surgery: implant reconstruction with silicone or saline-filled implants or flap reconstruction, which uses their own tissue from other parts of the body. Some women choose to “go flat” after surgery to remove one or both breasts. External breast forms can be used with this choice.
And it’s important to know that you don’t need to rush your decision. You can begin the reconstruction the same day as your mastectomy, or you can delay the decision for months or even years. Talk with your doctor and a plastic surgeon about your options.
This can vary from patient to patient, but generally you can expect to spend very little time in the hospital. Lumpectomies are usually outpatient procedures. Even with a mastectomy (unless you are starting breast reconstruction at the same time), you will likely spend no more than one night – if that. Of course, your overall recovery is going to take longer than that. After a lumpectomy, you should be able to return to normal activities within a week or less. But it may take a month to return to normal activities following a mastectomy and even longer if you have also already started reconstruction.
As part of the surgery for a mastectomy, your surgeon will insert small tubes at the site of the surgery. These drains keep excess fluid from building up in the empty space left by the surgery. These drains typically remain until the output slows – usually about two weeks – before being removed by your care team.
There are several reasons your doctor may suggest genetic testing before your surgery. There are certain genetic variants, including the well-known BRCA1 and BRCA2 genes, that are linked to increased risk for cancer – not just breast cancer. Some women with the BRCA genes choose to remove both breasts (even if one is currently unaffected by cancer) to avoid the risk of the disease in the future. Genetic details can help your care team make suggestions for monitoring and screening going forward. And the information can be valuable to your siblings or children, who may share your increased risk.
This content is not AI generated.
Are You Interested in Learning More?
Sign up for our e-newsletter for more tips and best practices from pediatricians.
Sign Up Here