Radiation Cancer Treatment Options
At Orlando Health Cancer Institute, patients have access to the most current, state-of-the-art cancer-fighting technologies. Our radiation oncologists specialize in treating specific types of cancer, working with medical oncologists and surgeons to deliver the most appropriate treatment for each individual patient.
This new technology gives Orlando Health Cancer Institute doctors a more precise and nimble way to treat lesions and tumors.
Ethos Therapy uses artificial intelligence to quickly analyze changes in your body from one treatment session to the next. These changes are then incorporated into your treatment plan, allowing for more precise targeting of your cancer.
This adaptive intelligence also minimizes your treatment time – in some cases, 30 minutes from start to finish – and reduces the potential for damage to healthy tissue.
Brachytherapy, also called internal radiation, involves the placement of radioactive material directly inside or next to a tumor. It uses a higher dose of radiation to treat a smaller area in less time than external-beam radiation. During the procedure, a radioactive seed is placed in a special plastic applicator, which is then laid over the treatment area for five to 10 minutes.
The following cancers we treat with brachytherapy:
- Gynecological cancers
- Breast cancer
- Head and Neck cancers
- Bronchus or airway cancer
- Skin cancer
- Prostate cancer
Radiation therapy uses high-energy radiation to shrink tumors and kill cancer cells. X-rays, gamma rays and charged particles are types of radiation used for cancer treatment.
The radiation may be delivered by a machine outside the body (external-beam radiation therapy), or it may come from radioactive material placed in the body near cancer cells (internal radiation therapy, also called brachytherapy).
Systemic radiation therapy uses radioactive substances, such as radioactive iodine, that travel in the blood to kill cancer cells.
About half of all cancer patients receive some type of radiation therapy during the course of their treatment.
For patients with thyroid cancer, I-131, or radioactive iodine, might be recommended if the cancer has spread to the lungs, lymph nodes or another part of the body. It also may be used to destroy any thyroid tissue not removed during surgery.
This treatment is effective because thyroid cells use nearly all of the iodine in the body to produce the thyroid hormone. When I-131 is administered orally by liquid or capsule, the thyroid cells absorb the radioactive iodine. This causes the cancerous thyroid cells, wherever they may be in the body, to stop growing.
In order to be effective, patients must have high levels of TSH, a thyroid stimulating hormone. To achieve a high level of TSH, it may be necessary to not take thyroid hormone pills for a few weeks. The loss of this medication will in turn cause the pituitary gland to release more TSH.
If abstaining from hormone therapy is not recommended by the patient’s physician, an injectable form of TSH called Thyrogen may be given. Patients receive this drug for two days and then have I-131 therapy on the third.
Patients who have I-131 therapy will give off radiation for a period of time. Depending on the strength of the dose, it may be necessary for patients to remain hospitalized for a few days in a special room to protect others from radiation. Other patients may not require any hospitalization. It is important after leaving the hospital that all I-131 patients follow strict instructions in order to protect others from radiation and to do so for the prescribed period of time.
Proton therapy is a form of radiation treatment which delivers a precise dose of radiation to tumors while sparing surrounding normal tissue. The result is a better option for treating some types of cancer while causing fewer harmful side effects.
Proton therapy, like all forms of radiation therapy, works by damaging the DNA of cancer cells, which may result in their growth arrest or death. Unlike X-rays, protons can be manipulated to release most of their energy within the tumor with little or no dose in the tissue outside the tumor; it is this feature of proton beams that may result in great potential benefit for select cancer patients.
For more information on our Center for Proton Therapy, visit www.OrlandoHealthCancer.com/Proton.
When cancer spreads, the liver is a common site for metastatic disease. Radioembolization (TheraSphere®, SIR-Spheres®) is an innovative therapy that delivers radiation directly to tumors in the liver.
TheraSphere®
TheraSphere® is a powerful, well-tolerated liver cancer therapy that consists of millions of small glass microspheres (20 to 30 micrometers in diameter, or about a third of the width of a human hair) containing radioactive yttrium-90. The product is injected by physicians into the artery of the patient’s liver through a catheter, which allows the treatment to be delivered directly to the tumor via blood flow.
This approach provides a high concentration of radiation treatment directed to the tumor, and limits both damage to surrounding healthy tissue and side effects for the patient that often result from other forms of cancer treatment, such as external radiation or systemic therapy (radioactive drugs). This form of radioembolization therapy also keeps future treatment options open as patients progress through the later stages of their disease.
SIR-Sphere®
SIR-Spheres® Y-90 resin microspheres are tiny radioactive ‘beads’ used in selective internal radiation therapy (SIRT), sometimes referred to as Y-90 radioembolization, and are used for the treatment of stage IV colon cancer that has spread to the liver and can’t be surgically removed.
SIR-Spheres® Y-90 resin microspheres therapy is a minimally invasive outpatient procedure, and patients usually go home hours after the procedure is completed.
SIR-Spheres® Y-90 resin microspheres are the only fully FDA-approved microsphere radiation therapy in the United States for the treatment of colorectal cancer that has spread to the liver.
Y-90 Treatment for Liver Metastasis
Y-90, also known as radioembolization, is used to treat tumors that originated in the liver or are metastasized to the liver from elsewhere in the body. For patients who are not a candidate for surgery or transplantation, Y-90 may be an option. The procedure may extend life from months to years and improve the patient’s quality of life. In some cases, it may eventually allow for the additional options of surgery or transplantation.
Tiny beads called microspheres are inserted by a catheter through a small incision in the skin and into the blood vessels in the liver which feeds the cancerous cells. The outpatient procedure typically takes an hour. These microspheres are tagged with the radioactive isotope yttrium Y-90. They then travel to the tumor site and are lodged in the tumor’s capillaries. Here they deliver a high dose of radiation to the tumor minimizing radiation to the remaining normal liver.
The radiation dose from the Y-90 microspheres will slowly decrease during the two weeks following the procedure and then disappear in approximately a month. The microspheres themselves will remain in the liver without causing discomfort or harm.
The technology that makes it possible to treat brain tumors with precision dosing using stereotactic radiosurgery (SRS) may also be applied to the treatment of tumors elsewhere in the body. This is called stereotactic body radiation therapy, or SBRT.
With this non-surgical procedure, delivery of radiation is accurate within 2 millimeters and at a very high dose, sometimes in a single treatment. The accuracy of the procedure enables the high dose because the oncologist is able to target the tumor while minimizing radiation to the surrounding, healthy tissue.
SBRT is an alternative to invasive surgery, especially for patients who are unable to have surgery due to the location of the tumor. The procedure may be used to treat malignant and benign tumors in the lungs, liver, spine and abdomen.
While many patients may be good candidates for a single treatment, the physician may recommend multiple treatments for others. This is especially true of larger tumors because healthy tissue must be protected from the dose of radiation needed for successful treatment. Delivering the required radiation during the course of two to five treatments allows for high doses to be delivered to the tumor while minimizing the effects of the radiation on surrounding tissue.
This very precise form of radiation is used to treat brain tumors and other neurological conditions. With stereotactic radiosurgery (SRS), the delivery of radiation is accurate within 2 millimeters. The non-surgical procedure delivers a very high dose of radiation, sometimes in a single treatment. The accuracy of the procedure enables the high dose because the oncologist is able to target the tumor while sparing surrounding, healthy tissue. SRS is an alternative to invasive surgery, especially for patients who are unable to have surgery.
While many patients may be good candidates for a single treatment, the physician may recommend multiple treatments for others. This is especially true of larger tumors because healthy tissue must be protected from the dose of radiation needed for successful treatment. Delivering the required radiation during the course of two to five treatments allows for high doses to be delivered to the tumor and the surrounding tissue to be preserved.
After treatment, patients may expect benign tumors to shrink during the course of two years or less. Malignant and metastatic tumors may shrink even more rapidly, sometimes as quickly as two months. Other tumors may stay stable and inactive rather than shrink, however the lack of growth benefits the patient and is considered a successful treatment.
Total skin radiation therapy, also known as total skin electron beam therapy (TSEBT), is used to treat mycosis fungoides, the most common type of cutaneous T-cell lymphoma. During the procedure, the skin surface is treated with low-energy electron beams from a linear accelerator. These electrons only penetrate the skin, sparing the body’s tissues and organs from radiation. Typically, the procedure is used in patients who are not responding to other treatments. It may be used in conjunction with other therapies. Patients may receive up to 12 daily treatments.
Xofigo, sometimes called radium 223 dichloride, is a radioactive drug used to treat patients with prostate cancer that has spread only to the bones and who are receiving treatment to lower their testosterone levels. Typically, this form of cancer has been resistant to medical or surgical treatment.
A decline in testosterone levels is important in these patients because testosterone may cause prostate cancer to grow. Patients who have had drug treatment to lower their testosterone levels, sometimes followed by surgery, and then experience the return of cancer are considered “castration-resistant.” Xofigo was developed for these patients. It is administered intravenously once every four weeks for a maximum of six doses. Clinical trials have shown that the treatment may extend life for up to 14 months.
Pluvicto is a targeted radioactive treatment for patients whose cancer has resisted hormonal therapy and chemotherapy. Using advanced imaging, our radiation oncologists can pinpoint cancer cells via telltale traces (PSMA, or prostate-specific membrane antigen) on the surface of those cells. Radioactive molecules are then sent to those cancer cells, largely avoiding nearby healthy cells.
Our Advanced Technology Options
Cancer treatment is a quickly advancing field with new technologies bringing both improved treatment effectiveness and enhanced patient safety. Orlando Health Cancer Institute invests in groundbreaking technologies that continue to move cancer treatment forward. Listed below are some of the systems our doctors use to provide accurate, safe therapies that may also reduce patient treatment times.
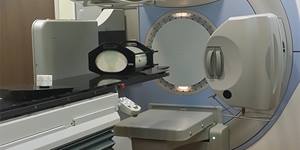
With over 5,000 installed sites worldwide, the high-performance Clinac® is a reliable accelerator built on the proven C-series platform. Designed to deliver a wide range of imaging and patient treatment options, the Clinac system offers advanced features to facilitate state-of-the-art treatments including IMRT, IGRT, VMAT, RapidArc and stereotactic radiosurgery. With an eye toward the future, every Clinac machine is built to be supported and upgraded, enabling it to stay ahead of the curve. Varian’s On-Board Imager (OBI), high intensity mode, RapidArc, RPM gating and motion management tools help deliver fast and effective patient treatments with accuracy.
Available in Clermont
Elekta Synergy system was the first linear accelerator to bring 3D image guidance into the treatment set up process. The system is equipped with imaging tools that help clinicians visualize tumor targets and normal tissue, and their movement between and during fractions. The integration of this technology in the Elekta Synergy gantry enables physicians to perform imaging with the patient in the treatment position at the time of treatment, to optimize patient setup before therapy.
Key imaging tools include 2D, 3D and 4D volumetric cone-beam imaging for soft tissue visualization; 2D real-time, fluoroscopic-like imaging for targets that move frequently; and 2D kV imaging for standard and orthogonal planar imaging.
The MEVION S250 Series™ is based on unique core technology. Unlike other systems, Mevion’s proton therapy systems have been engineered to eliminate the complexity of large accelerators and long beam transport lines. Mevion has designed the world’s only gantry mounted superconducting proton accelerator. Powered by the TriNiobium Core™, this revolutionary proton accelerator is only 6 feet (1.8 meters) in diameter, but can generate 250 MeV protons capable of reaching targets as deep as 32 centimeters.
The TomoTherapy treatment system delivers radiation therapy with a spiral delivery pattern (TomoHelical™) or discrete-angle approach (TomoDirect™). Photon radiation is produced by a linear accelerator that travels around the patient and moves in unison with a device called a multi-leaf collimator that shapes the beam. Meanwhile, the couch is also moving—guiding the patient slowly through the center of the ring.

The Varian Edge™ Radiosurgery System offers advanced tools designed to deliver highly accurate radiation to tumors of the brain, spine, lungs and other areas of the body.
In addition to the high level of confidence in targeting tumors with precision, the Edge system also offers enhanced power and speed. This allows our surgeons and clinicians the ability to pinpoint the target and deliver highly focused treatments, in fewer sessions and at a faster rate, while minimizing the radiation dose received by surrounding healthy tissue.
By being able to pinpoint the tumor and track it in real time, Edge’s real-time system design helps enable a high level of synchronization between imaging, patient positioning, motion management, beam shaping and dose delivery technologies — all potentially reducing the overall time and resources required when compared to traditional methods.
Ethos Therapy is radiation therapy that uses artificial intelligence to boost its flexibility, accuracy and efficiency. After quickly analyzing images of your body at the start of each session, the AI-driven therapy makes rapid adjustments to your day’s treatment plan. Ethos therapy offers several benefits for patients:
- Treatment changes are done quickly, keeping sessions at an hour or less.
- Precision treatment means less radiation exposure to healthy tissue.
- Your tumor or lesion can be more precisely targeted to reliably destroy cancerous cells.

Available in Lake Mary and Ocoee
High-Precision Radiotherapy Treatment
Designed from the ground up to treat moving targets with advanced speed and accuracy, the TrueBeam platform is a fully-integrated system for image-guided radiotherapy and radiosurgery. TrueBeam treats cancer anywhere in the body where radiation treatment is indicated, including lung, breast, prostate and head and neck.
The carefully guided, automated workflow on the TrueBeam system uses intuitive visual cues to enhance safety and reduce patient treatment times. Streamlined imaging and patient positioning tools enable more flexibility to treat cancer throughout the body. Having the power to not only treat quickly, but to deliver high, accurate dose rates are hallmarks of the TrueBeam system.
Navigate Your Health


Find a Cancer Physician
Find a Cancer Physician
Meet our doctors who specialize in the full range of cancer care. Our team of experts has experience in a variety of specialty areas. Together, we provide comprehensive evaluation, diagnosis and treatment options.
Learn More

Patient Portal
Patient Portal
If you are a patient at Orlando Health Cancer Institute, our free online patient portal provides an easy and secure way to manage your health information. Reach us from any location at a time that’s convenient for you.
Learn More

Virtual Visit
Virtual Visit
Need to talk with a doctor, but don’t want to leave your home? Try our virtual visit (telehealth) option to connect with a physician from your phone, tablet or computer.
Learn More
